Discover the 5 key facts about the Child Pugh score, a powerful tool used to assess liver disease severity, prognosis, and treatment strategies.
Understanding the Child Pugh Score:
Evaluating liver function has long become an essential role in diagnosing several patients with chronic diseases through use of the Child-Pugh score by doctors. Child Pugh scoring gives an acceptable way of judging the intensity of chronic liver disease such as cirrhosis while relating it to the prediction and treatment options. Let us read more about what Child Pugh scores are, how they operate and what role they play in the medical profession.
What Is the Child-Pugh Score?
The Child Pugh score is a clinical scoring system that helps doctors evaluate the prognosis of patients with liver disease. It was initially developed in 1964 by Drs. Child and Turcotte and later modified by Pugh in 1973 to its current form. This score evaluates the functional capacity of the liver in patients with chronic liver disease, particularly cirrhosis, by examining five key factors:
1. Bilirubin level:
Reflects the ability of the liver to excrete bile.
2. Albumin level:
The liver makes a very important protein in the body, called albumin.
3. Prothrombin time or INR:
It gives the degree of coagulability of blood.
4. Ascites:
Presence of fluid in the abdomen
5. Presence and severity of hepatic encephalopathy:
The brain gets confused because of failure of the liver
How Is the Child Pugh Score Calculated?
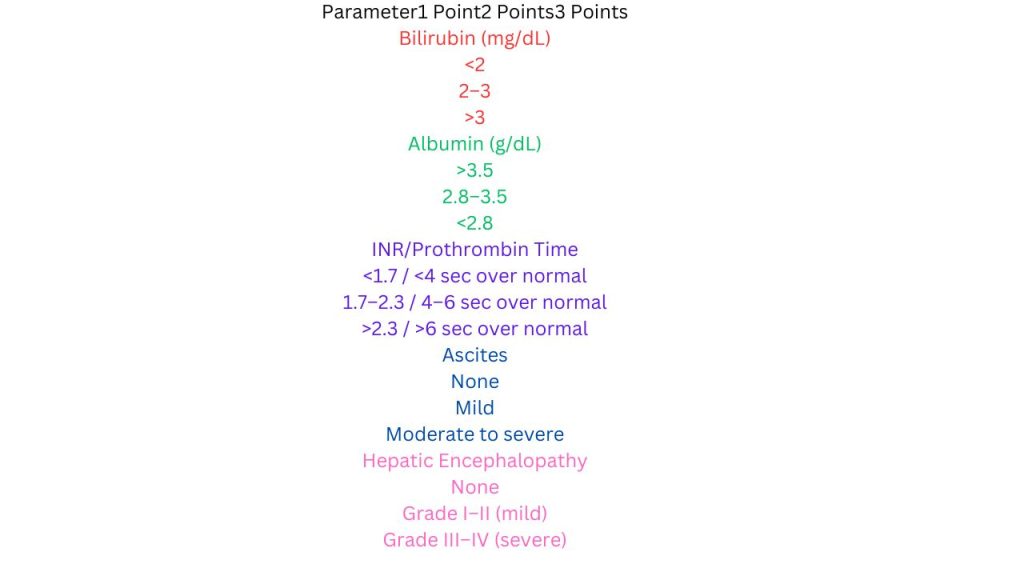
The scoring system is straightforward and involves assigning points based on the severity of the five parameters:
| Parameter | 1 Point | 2 Points | 3 Points |
| Bilirubin (mg/dL) | <2 | 2–3 | >3 |
| Albumin (g/dL) | >3.5 | 2.8–3.5 | <2.8 |
| INR/Prothrombin Time | <1.7 / <4 sec above normal | 1.7–2.3 / 4–6 sec above normal | >2.3 / >6 sec above normal |
| Ascites | None | Mild | Moderate to severe |
Hepatic Encephalopathy | Not applicable | Grade I–II; mild | Grade III–IV severe
After adding up the points from each parameter, the total score categorizes the patient’s liver function into one of three classes:
– Class A (5–6 points): Mild liver disease with good prognosis.
– Class B (7–9 points): Moderate liver disease with intermediate prognosis.
– Class C (10–15 points): Severe liver disease with poor prognosis.
Clinical Significance of the Child Pugh Score
The Child Pugh score has the following important applications in the management of chronic liver disease:
1. Prognosis
The score predicts the survival time of patients with cirrhosis. For instance:
– Patients in **Class A** have the best survival rates, with an average 1-2 year survival of 85-90%.
– Patients in **Class C** have significantly poor survival, and it is less than 35-45% at surviving 1-2 years.
2. Treatment Planning
The score helps physicians design treatment strategies. For example:
– Patients in **Class A** may tolerate treatments that are aggressive like surgical intervention or liver transplantation.
– Patients in **Class C** are usually managed on a palliative approach, given their poor reserve.
3. Liver Transplant Evaluation
The Child Pugh score is one of the tools used to prioritize patients for liver transplants. Those with severe liver disease (Class C) are generally given higher priority.
4. Medication Dosing
Patients with higher scores are more likely to have impaired liver metabolism, necessitating careful adjustments in medication dosages to avoid toxicity.
Limitations of the Child-Pugh Score
Although the Child Pugh score is commonly used, it has a number of drawbacks:
1. Subjective:
Ascites and hepatic encephalopathy are subjective factors that may be subject to the observer’s discretion. This results in a lack of homogeneity in the scoring process.
2. Not Comprehensive
This score does not incorporate all parameters influencing the prognosis of the disease. The renal functions and other comorbid diseases like infections and cancer are not considered in the scoring process.
3. Obsolescence in Certain Respects
As scientific discoveries in medical sciences progress, newer scores have been evolved. More recently, there are the MELD score or Model for End-Stage Liver Disease scores. In comparison with Child-Pugh scores, it uses much more objective parameters: bilirubin, INR, and creatinine, and has been rated better in terms of predictability of survival in those on the transplant waiting list for liver disease.
Although the Child-Pugh score is useful, the **MELD score** has been more recognized lately, especially for transplant allocation. Differences:
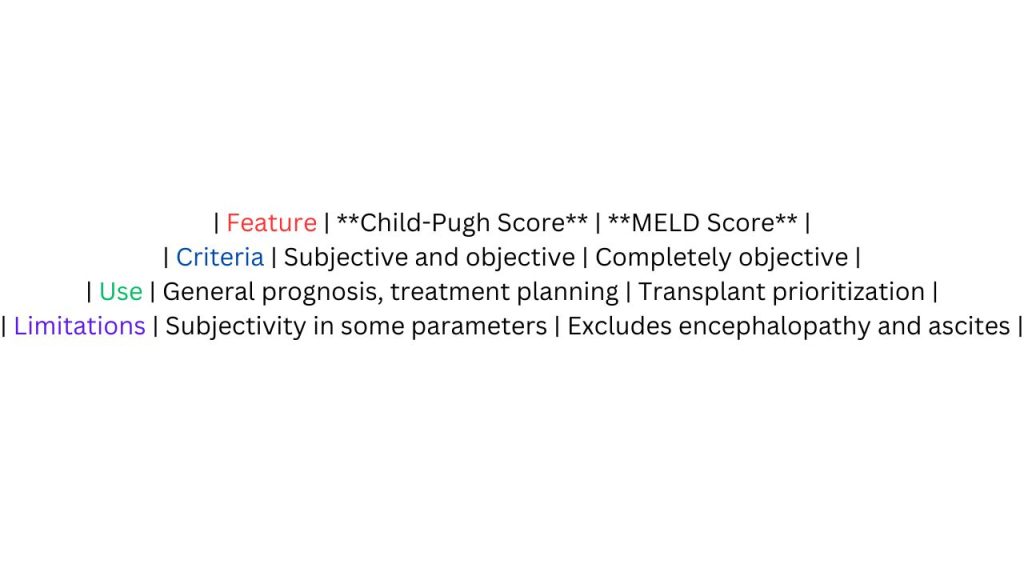
| **Feature** | **Child-Pugh Score** | **MELD Score** |
| **Criteria** | Subjective and objective | Completely objective |
| **Use** | General prognosis, treatment planning | Transplant prioritization |
| **Limitations** | Subjectivity in some parameters | Excludes encephalopathy and ascites |
Despite the rise of the MELD score, the Child-Pugh score remains widely used because of its simplicity and effectiveness in day-to-day clinical practice.
Real-World Applications
Case 1: Assessing Liver Cirrhosis
A 55-year-old patient with chronic hepatitis C presenting in jaundice, mild ascites, and confusion has the following laboratory values: bilirubin of 2.5 mg/dL, albumin of 3 g/dL, and INR of 1.8. Applying the Child Pugh score:
– Bilirubin = 2 points
– Albumin = 2 points
– INR = 2 points
– Ascites = 2 points
– Encephalopathy = 2 points
Total score = 10, placing the patient in **Class C**. This is severe liver disease, and discussions around listing the patient for a possible transplant occur.
Case 2: Intraoperative Decision Making
Patient with cirrhosis aged 63, has to undergo abdominal surgery. Calculated Child Pugh score is **Class B**. This middle classification has placed the risk intermediate. The surgical team therefore ensures extreme caution and performs possible optimization before surgery. Read about can bad news make you sick.
Conclusion:
The Child Pugh score is an essential tool in the management of liver disease, offering a simple yet effective way to assess liver function and predict outcomes. While it has limitations and is gradually being supplemented by newer scoring systems like the MELD score, its clinical relevance remains undeniable. For patients with chronic liver disease, this scoring system often guides treatment decisions, enabling personalized care that balances prognosis with quality of life.
If you, or someone close to you, have been diagnosed with a liver disease, tools such as the Child Pugh score can empower you to have informative discussions with your healthcare team and take proactive steps in managing health.